http://straightupdoc.com/?p=175
Q: My dentist recommended a “deep cleaning” (scaling and root planning). Do I really need this?
Short Answer: Maybe
Long Answer:
When reading comments online and hearing concerns from patients, issues revolving around deep cleanings are some of the most common. But hold on to your hats, this is going to be a doozy. If you don’t want all the nitty-gritty about deep cleanings, stop now and go back to whatever else you were doing. This subject takes some work to do it justice.
WHY ARE DEEP CLEANINGS RECOMMENDED AT ALL:
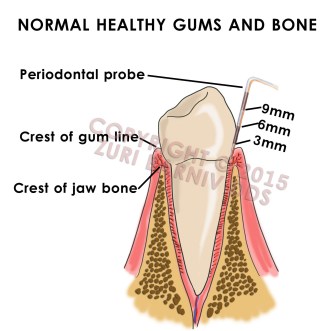
Healthy gums are tight, pink and don’t bleed when they are brushed or flossed. A dentist or hygienist can take a little ruler called a periodontal probe and measure the depth of the pocket of gum that forms near the base of your tooth. A measurement of 1-3mm with no bleeding is considered healthy and normal.
Normal gums and jaw bone. Notice the probe is measuring less than 3mm in pocket depth and the gums appear pink and hug the tooth tightly.
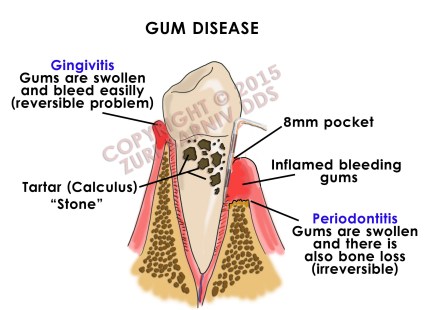
When teeth are surrounded by a constant irritant like food debris or plaque (the soft white film that you can scrape off with your fingernail), the gums swell a little and they tend to bleed easily. Because the gums swell slightly, it makes the pocket of gum seem deeper and it may be 4-5mm in depth. This is called gingivitis and it is reversible. But if the soft white plaque is not properly removed for a few days, it begins to mineralize into a hard cement-like substance called tartar (“calculus”, also known in other countries as “stone”.) Tartar cannot be removed with a regular toothbrush or by flossing. Over time, tartar builds up under the gums where it can be difficult to see, and this creates a constant irritation to the gums and bone it contacts. Ultimately, the jaw bone holding the teeth tends to “melt” away. This gradual, non-reversible bone loss is called “periodontitis” and this will be reflected in even deeper pocket depth (usually exceeding 5mm). Again, to clarify, if there is no actual loss of bone and only the gums are red and inflamed, the condition is called “gingivitis”.
Although bone loss is a key component to periodontitis, the term is surprisingly not perfectly defined and two dentists can look at the same patient and come to different conclusions. That’s because a dentist uses a combination of periodontal probing measurements, x-rays, clinical observation and their experience to make the diagnosis. If, however, periodontitis is diagnosed, it is common to recommend a deep cleaning as a first step. Subsequent steps may include surgical intervention. If periodontitis continues unabated and untreated, the teeth affected could eventually become loose, painful or fall out. This is because the support structure for the teeth (your jaw bone) is no longer present in sufficient quantities. See the figures below:
This shows both gingivitis (swelling of the gums) and periodontitis (a more advanced state where bone loss occurs)
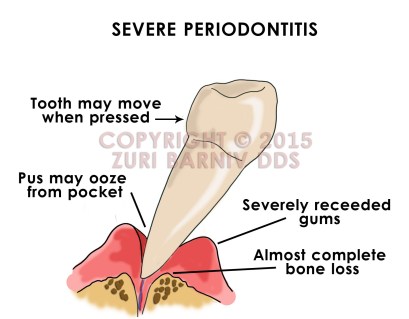
This is the most severe form of periodontitis. There is basically no more bone holding the tooth in the jaw and the gums bleed easily when touched. Some people may see pus coming out of the gum pockets when pressed. Teeth in this state tend to move more easily and some people report noticing their teeth have “shifted” from their original position.
In addition to losing teeth, many studies point to evidence that periodontitis can exacerbate or trigger problems throughout the body. There have been links to arthritis, diabetes, heart disease, stroke and more. Obviously that doesn’t mean periodontitis causes these things directly, but it is thought that chronic inflammation in the body can trigger or exacerbate other medical conditions. There is even a link between gum disease (periodontitis) and pregnancy-related problems like pre-term deliveries, miscarriage, low birth weight and other issues. It is important to remember that the surface area of the gums in your mouth is about equivalent to that found on the palm of your hand. Imagine if your palm was red, inflamed and bled when you touched it. One would think that would be reason enough to seek treatment. Clearly, periodontitis is a serious problem with potentially serious consequences.
SO WHAT IS A DEEP CLEANING?
A deep cleaning, also known as scaling and root planning (SRP), is the procedure which removes the deposits (tartar) under the gums which cause the chronic irritation and bone loss. In a SRP procedure, not only are deposits removed from the root surfaces, but those surfaces are then smoothed (planed) so they become more resistant to further buildup. Sans surgical intervention, the bone lost will never regenerate and this is why many authorities consider periodontitis a treatable but incurable disease. Since deep cleanings require the dentist or hygienist to clean under the gums, most people find the experience too painful to do without anesthesia. It is very common to have one half of the mouth cleaned at a time. After two visits, the process is complete. It is then recommended that the patient return every 3 or 4 months for a “maintenance” procedure. This assures the dentist that the tartar is kept from reforming under the gums and evidence that the therapy was effective is gathered. It is not uncommon for dentists to also make a referral to a gum specialist (a periodontist) to further evaluate and treat periodontitis.
WHAT DOES IT ALL MEAN FOR THE YOU?
I agree with the merits of a deep cleaning and I, occasionally, recommend it to my patients. The unfortunate thing is that many practitioners use this service to augment their bottom line and the patient is powerless to know if the recommendation was warranted or not. Remember in the above discussion that the term “periodontitis” is not defined in stone. It is diagnosed by looking at many different things. Some dentists define periodontitis so liberally that nearly all their patients are recommended this procedure. But most dentists use guidelines set by insurance companies to define periodontitis and the need for a deep cleaning. In other words, if the insurance company would agree to pay for the procedure, the dentist is likely to recommend it. Most insurance companies expect pocket depths to be more than 4mm and across several teeth in each quadrant of the mouth before they agree to cover a deep cleaning. Most insurance companies also require a copy of recent x-rays and a written diagnosis to approve the procedure. But even with x-rays, the pocket measurements are somewhat subject to interpretation and to the specific operator. Combined with the fact that there is a large financial interest in doing a deep cleaning over a regular cleaning, the operator may be motivated to use the most liberal of interpretations when probing pockets. This may not be in your best interest. To illustrate these points, we will look at two scenarios:
Scenario #1:
Trevor, who hasn’t been to a dentist for “several years”, comes to the dental office for a “check up and cleaning”. The dentist completes an exam, x-rays, evaluates the pocket depths and the overall health of his gums. Since Trevor hasn’t been seen by a dentist in quite a while, he has some plaque and calculus (tartar) around his teeth and in some areas where it cannot be seen easily, but it is minimal. In looking at the x-rays, the dentist confirms some of what he saw in the exam and confirms the problems are present but localized to a few areas. The dentist completes a full mouth probing and finds that Trevor has a few back teeth with 4mm and even 5mm pockets. The dentist also notices that some areas bleed slightly when he does the probings. The dentist decides to take a more relaxed approach and proceed with a regular cleaning (prophylaxis). He advises Trevor to return in 6 months to recheck the areas and to look for signs of chronic and persistent problems. The dentist receives about $100 when his hygienist does this simple cleaning, it takes an hour to do it and the office will earn another $100 in 6 months when Trevor returns for his second cleaning. Since the hygienist is paid $50 per hour, the office makes a profit (before non-salary expenses) of about $50 for this cleaning.
Scenario #2:
Trevor goes to a different dentist under the same circumstances. In this case, the second dentist makes a different judgment call and recommends a full mouth deep cleaning (four quadrants of SRP). The hygienist completes this service in about three hours which is spread over two appointments and the office collects $1,000 for the procedure. As is customary after a deep cleaning, Trevor is instructed to return in 3 months for a maintenance procedure which costs about $150 (maintenance procedures cost more than regular cleanings and are recommended more frequently). In this scenario, the office took three hours to make a $850 profit in the time they would normally make $150 ($50 x 3 hours) with regular cleanings. Furthermore, Trevor is now expected to return every 3 months for a maintenance procedure which translates to a $100 profit at each appointment (as opposed to $50 for regular cleanings). Since this procedure is recommended much more often than a 6 month cleaning, the office makes a $400 profit the following year as opposed to $100 when only considering the “maintenance” Trevor will need.
THE MONEY-MAKING DEEP CLEANING:
The numbers add up quickly: Over two years, the dentist in the first scenario doing only regular cleanings made $400 using 8 hours of his hygienist’s time ($50/hour profit). The dentist in the second scenario doing a deep cleaning made $1,550 using 10 hours of his hygienist’s time ($155/hour profit). So when a dentist is looking in Trevor’s mouth and deciding on the diagnosis to make, it becomes extremely tempting to choose the path which assures a much greater profit. Most patients would assume that the licensing authority, dental society or even the insurance companies would catch a dentist who over-recommends SRP. Unfortunately, that assumption would be wrong. One reason is that measuring pockets is time-dependent and, as discussed previously, is relatively subjective in nature. For example, a dentist accused of recording pockets deeper than they actually were could say the gums were particularly swollen on the day the readings were done. That would be nearly impossible to disprove. Also, when measuring pockets, the ruler used is typically based on 1mm increments (see the first figure at the top of this post). Dentists are typically taught to round up not down. If a pocket is 3.5mm deep, the dentist will almost always record it as 4mm. That could be the difference between “healthy” and “diseased”. Also, there is quite a lot of difference in how pocket measurements are done. Some practitioners push really hard and others use a very gentle touch. A firm hand will cause the ruler to go further into the gums which will give the impression that the pocket was deeper than was recorded by the gentle operator. Firm probing is also more likely to make the gums bleed, again, reinforcing the diagnosis of periodontitis. Even x-rays can be misleading, giving the illusion that there is no bone loss, when in fact, there is, and vice versa. That is because x-rays look at 3-dimensional objects in 2-dimensions. This is why some insurance companies don’t require x-rays at all and why a dentist can claim a diagnosis of periodontitis without any objective evidence. Unless the situation is overtly fraudulent and the dentist is diagnosing periodontitis for every single patient, it will be nearly impossible to prove any nefarious intentions. Some unscrupulous dentists take advantage of this situation and convince patients they need a deep cleaning when, in fact, it is totally unjustified. I have seen this more times than I wish I had…
A PATIENT’S PERSPECTIVE:
Since a deep cleaning is relatively invasive, it is my opinion that any dentist who recommends it without genuine need is behaving unethically. There is nothing worse than taking advantage of someone’s lack of knowledge for profit and these situations are extremely troublesome.
In my office, if a patient has a few 4mm or 5mm pockets, some bleeding gums and a little bone loss in isolated locations, I don’t rush to recommend a deep cleaning. Typically we start with a simple cleaning and have the patient return in 6 months or less. At that appointment we evaluate the situation again. If the buildup of tartar under the gums is persistent, there is still bleeding and the areas we worked on have not improved, we will have a discussion with the patient about the merits of SRP. We will review the risks, benefits and alternatives before making a decision together. Sometimes we decide to wait another 6 months, sometimes we recommend they see a periodontist (gum specialist) and sometimes we elect to do SRP.
If a new patient comes to my office who hasn’t seen a dentist in a few years, there is calculus under the gums throughout their mouth, many deeper pockets in excess of 5mm, obvious bone loss and bleeding on probing throughout the mouth, we will recommend SRP or refer them to a periodontist. In this case, I believe (remember, this is all dentist-specific) the recommendation is justified. Sometimes patients that clearly need SRP will ask to postpone the procedure and to instead get a simple cleaning. This is usually discouraged. If only the areas above the gums are cleaned (this is what’s done in a simple cleaning) and calculus remains under the gums, this can cause the top part to heal and the deep parts not to. In the worst case, this can lead to a gum infection which can then lead to more serious issues. Ironically, these are cases where it is better to do nothing than to do a simple cleaning (if those were the only options).
There are some important things to keep in mind if a deep cleaning is recommended and a decision to proceed is made. Most patients cannot tolerate the procedure without local anesthesia because the work happens fairly deep under the gums. Suspicions should be raised about the quality or need for SRP if very little or no anesthesia was required to complete the procedure (unless you know yourself to be quite pain tolerant). Time is also a factor in assessing the quality of the work completed. A deep cleaning is labor intensive and requires a substantial amount of time to complete. This is why more suspicions should be raised if a dentist suggests doing all four quadrants (the entire mouth) in one visit or if the procedure takes too little time to complete. A reasonable amount of time to do half the mouth would be 90-120 minutes. If the dentist or hygienist is able to complete half a mouth of SRP in less than 75 minutes, this is usually a sign that all or part of this procedure was never needed or that the procedure was done poorly. I recommend asking the office how long the procedure will take before committing to it – some judgments can be made based on the answer.
Keep in mind that when SRP is done correctly, there are multiple injections of anesthesia involved (four, five or more injections is not uncommon). Usually, half your face (either right or left) will be numb and most patients find the experience to be quite unsettling and somewhat exhausting. The process of removing calculus under the gums can be intense and many patients describe it as the hardest part of their dental treatment (when compared to crowns, fillings and even extractions). Some patients find it to be a much better experience if they are lightly sedated either with nitrous oxide (laughing gas) or with pills (valium, triazolam, etc.). SRP is also challenging for the patient because of the time involved and the significant amount of “scraping” required to remove all the calculus and smoothing of the root surfaces. Naturally, patients respond to treatment differently and some people find the experience to be no problem at all. But since most people find it intense, it would raise some concerns in my mind if nearly everyone in a dental practice was getting deep cleanings that they described as relaxing and easy. There will always be those patients that are highly tolerant of medical procedures with high pain thresholds, but they are not in the majority.
The latter description sounds rather awful to most people, which is why we don’t recommend SRP lightly to anyone. Nevertheless, if a patient genuinely needs it, there is simply no other way to circumvent the problem but to do SRP. This is why I discourage patients from automatically assuming a recommendation for SRP is just a money-making tactic or some sort-of gimmick. When indicated and properly performed, SRP is an important step towards improving total health as well as keeping teeth longer and healthier. It is worth doing under the right circumstances and this point cannot be overstated.
CONCLUSION:
It is a patient’s right to understand why a recommendation for a deep cleaning is being made. It is helpful to have the dentist point out the calculus and bone loss on the x-rays (which can be seen in the majority of cases).The dentist should also freely share the full mouth probing and explain where deeper pockets were found and how they relate to the general health of the gums. If the dentist or hygienist never recorded pocket depths at all, then this further raises suspicions of how the diagnosis was made. Some more advanced cases can be easily diagnosed with x-rays alone, but most cases require a full mouth probing as well. Independently of the dentist, if you see blood every time you brush, this adds support to the diagnosis of periodontitis. It is always appropriate to ask the dentist to explain why he or she recommended a deep cleaning as opposed to something simpler. If in doubt, I always recommend getting a second opinion.
Once a deep cleaning is done, maintenance is an important step to keeping things healthy; however, I do not believe that maintenance procedures need to be continued indefinitely for everyone. The topic of maintenance and the need for it will be covered separately.